Big breakthroughs may restore a sense of touch to U.S. military personnel who have lost limbs in service of the country.
U.S. forces suffered 6,144 traumatic amputations between 2000 and 2011, according to research conducted by the Armed Forces Health Surveillance Center -- and more than 2,000 of these were major amputations involving the loss of a hand, foot or more.
Junior enlisted Army and Marine Corps members in combat-specific positions have experienced the most of these amputations. Increased frequency and intensity of ground combat operations in Iraq and Afghanistan are often cited for the increase.
There have been tremendous advances in prosthetic limbs in recent years but few ways to interface tissue with tech, meaning those innovations can't be fully exploited.
Could that all be changing?
Brains or bodies?
The Reliable Neural-Interface Technology (RE-NET) program from DARPA, the Pentagon's advanced research group, has a vision: direct, reliable connections between prosthetic limbs and the brain, spinal cord, and neurons in replacement limbs.
DARPA has made some highly publicized breakthroughs in interfaces straight to the brain, but many believe practical applications are unfortunately not in the immediate future.
However, there is near-term realistic hope in new neural-interface technologies.
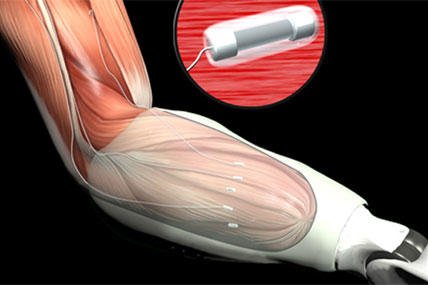
"Peripheral interfaces" use signals from nerves and muscles to control prosthetics and provide direct sensory feedback. Combining man and machine through these nerve and muscle hook-ups looks far more promising for transforming the lives of amputees in the near future.
"Because implanting them is a lower-risk, less invasive procedure, peripheral interfaces offer greater potential than penetrating cortical electrodes," said DARPA program director Jack Judy. "RE-NET program advances are already being made available to injured warfighters in clinical settings."
One key challenge to fully integrated prosthetics is the specific connection between tissue and electronics. Some prototypes plug into the nervous system directly at the spinal cord; others connect in through the peripheral motor system.
In order to make the motor control links seamless between the human and the replacement limb, DARPA is also unraveling how information about limb movements travels through neural tissues and implanted interfaces.
Long-term links between brains and tech
Part of the RE-NET team, The Rehabilitation Institute of Chicago has developed and demonstrated one living peripheral-nerve interface.
Called micro-targeted muscle re-innervation or TMR, this type of interface forms a long-term connection that lets the wounded warrior communicate, direct and control movement of the artificial limb.
Simply put, TMR lets those with upper-arm amputations undergo a surgery that will allow them to direct and control their prosthetic device by just thinking about it. It could be described as rewiring a person's nerves.
The Institute's surgical procedure reassigns to the pectoral muscles the nerves that once controlled the arm and hand. The new interface then allows existing muscles to control the prosthetic.
After the surgery, the patient returns home and waits five to six months for the nerves to regrow. An arm is then custom-built to correspond to the newly re-innervated muscles.
Army Staff Sergeant Glen Lehman, who was injured in Iraq, recently showed off a very successful TMR procedure, which gave him such control that he can capture a fine gauzy fabric as it drops through the air, grab a coffee cup, and even grasp a ball.
This radically innovative procedure is now available to the public.
To be eligible and benefit from TMR surgery, a rigorous medical review is conducted. The hospital looks at eligibility criteria including that the candidate must be at least 14 and have an amputation above the elbow or at the shoulder within the last 10 years.
But how do you feel?
Can a state-of-the-art robotic arm give that combat veteran back the sense of touch, however -- with manmade fingers?
FINE is another nerve interface technology showing promise in the RE-NET program. While TMR improves control, FINE focuses on restoring the sense of touch.
FINE (flat-interface nerve electrodes) interfaces with residual nerves in the patient's partial limb; in the system, electrodes are placed around individual peripheral nerves and used to record motor-control information.
This direct sensory feedback system means a patient can feel a light switch in the dark, find a bus pass buried in a bag and just generally grasp things without having to directly look at them.
What's next?
In 2012, DARPA invested $24 million into this promising technology. This year the agency will spend a further $10.2 for human testing and FDA applications, and to develop a 28 degree-of-freedom avatar.
As the RE-NET program continues, it is hoped that even better limb-control and sensory-feedback capabilities from neural interface technologies will emerge and become widely available in the future.
Not only does RE-NET have potential for injured service members, it has promise to aid the wider civilian community with medical amputations, spinal cord injuries, and neurological diseases.